Gastroparesis is a condition where the stomach doesn't empty properly. This causes symptoms like nausea, vomiting, bloating, weight loss, and leads to more serious health conditions.
Gastroparesis can be caused by many different conditions, but most cases are idiopathic, meaning there is no known cause.
This article will help you understand what gastroparesis is, potential causes, common symptoms, how to diagnose it, and how to treat it.

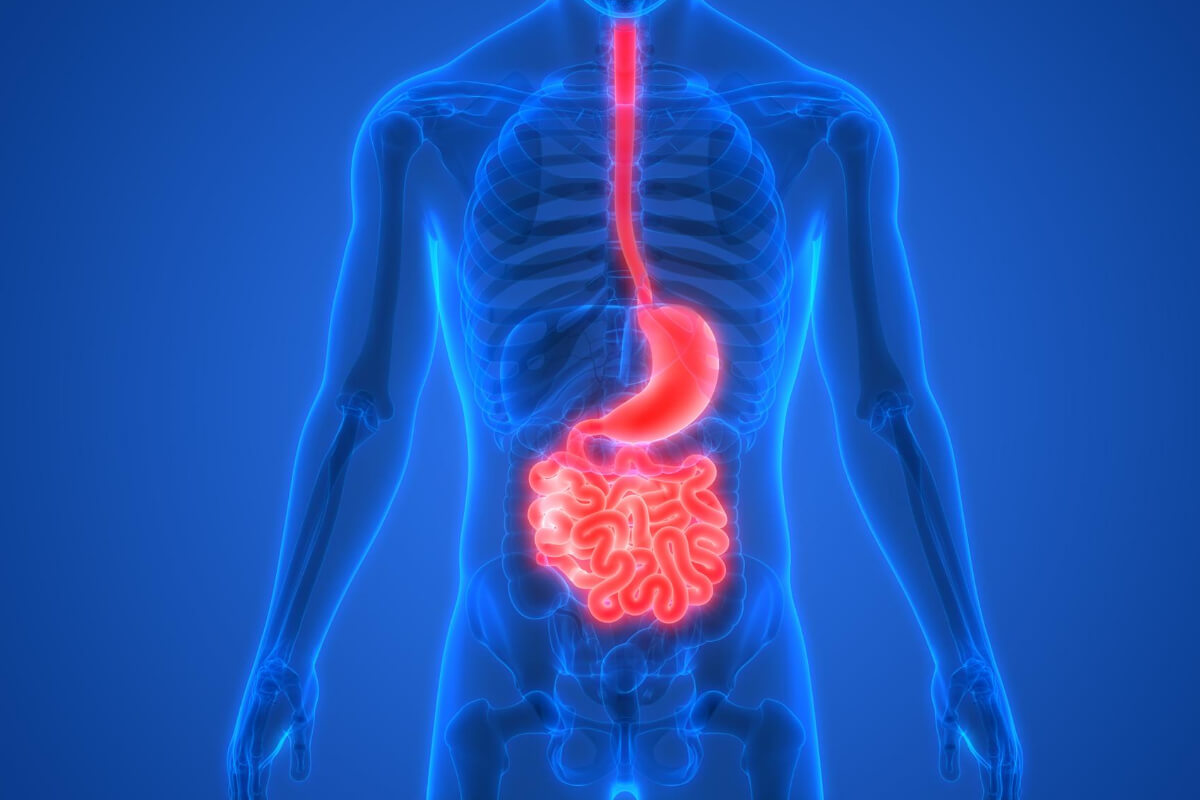
What Is Gastroparesis?
Gastroparesis occurs when your stomach isn't emptying properly and food is staying in your stomach longer than it should. When functioning correctly, the vagus nerve and stomach muscles will usually contract to help push food down into the intestines.
When gastroparesis happens, food stays in the stomach longer than normal due to damaged wall muscles and nerves. That leads to content moving slowly through the digestive system or not at all.
What Causes Gastroparesis?
There are many different factors that can contribute to gastroparesis. One of the most common causes of gastroparesis is damage to the vagus nerve, which controls the stomach muscles that move food into your small intestine.
Other causes of gastroparesis include:
- Diabetes.
- Cancer treatments.
- Diseases affecting the nervous system, such as multiple sclerosis.
- Medical conditions like anorexia and bulimia.
- Medications such as narcotic pain medications, some antidepressants.
- Surgery that involves the stomach, small intestine, or esophagus.
- Metabolic conditions such as hypothyroidism.
- Viral stomach infections such as gastroenteritis.
What Are the Symptoms of Gastroparesis?
The main symptom of gastroparesis is delayed gastric emptying. Gastroparesis symptoms vary depending on the severity of the disease, which can make diagnosis more difficult.
Some people with mild gastroparesis may have only minor symptoms while others may experience severe complications.
Gastroparesis symptoms include:
- Nausea
- Vomiting
- Bloating
-
Weight Loss
-
Abdominal pain
-
Poor appetite and feeling full constantly (early satiety)
-
Acid reflux
-
Poor blood sugar level management
What Are Complications Can Develop From Gastroparesis?
If left untreated, gastroparesis can lead to more serious problems. Some of these complications include:
Bacterial Overgrowth
Bacteria will grow in the stomach and the gut bacteria balance because the food is not being digested properly. That can lead to small intestinal bacterial overgrowth (SIBO) or other gastrointestinal issues.
Diabetes and Blood Sugar Changes
People who develop gastroparesis often struggle with their diabetes management. They may need to adjust their insulin doses or take additional medication to control their blood glucose levels.
Bezoars
The undigested food can block the stomach's pyloric sphincter, which prevents the stomach from emptying completely. This can lead to a buildup of hard lumps called bezoars in the stomach. Bezoars can also block the small intestine, causing nausea, vomiting, and abdominal pain.
Malnutrition and Undesired Weight Loss
If the food is not breaking down and digesting, your body is not getting the nutrients from the food you're eating. That can lead to unwanted weight loss and lack of nutrients to keep your body healthy.
How Is Gastroparesis Diagnosed?

A doctor will typically start by looking at your medical history, performing a physical exam, asking about your symptoms, and ordering various tests.
Tests that are performed can include:
- Blood Tests - Tests to look at blood sugar levels, dehydration, infection, or malnutrition problems.
- Barium X-ray - Barium will coat your stomach, esophagus, and small intestine, so that it will show up in your x-rays. After fasting for 12 hours, if it shows that food is still in your stomach, then you will probably have gastroparesis.
-
Gastric Emptying Scintigraphy - You will eat food that contains a small radioactive tracer. Your doctor will use this test to see how quickly the tracer moves through your digestive tract. If there is more than 10% of the food left in your stomach 4 hours after eating, then you likely have gastroparesis.
- Smart Pill - The Smart Pill is a tiny electronic device the size of a pill that you swallow. It measures the time it takes to move through your body until it exits in your stool. These measurements help doctors understand whether your stomach and digestive tract are working normally.
- Ultrasound - Using high-frequency sound waves, the doctor can rule out other diseases like gallbladder disease or pancreatitis.
- Upper Gastrointestinal Endoscopy - A tube with a camera on the end is inserted into your mouth, throat, esophagus, and stomach to take images. The doctor uses this technique to examine your upper GI tract for food remains or a bezoar.
Gastroparesis Treatment
There are several different treatments available for people with gastroparesis. There are no cures for gastroparesis, but some treatments can improve your quality of life and treat underlying conditions.
Medication
There are some medications that may help reduce symptoms and prevent complications. Medications used to treat gastroparesis symptoms include:
- Metoclopramide (Reglan) - Metoclopramide works by relaxing muscles in the gut, and encouraging them to contract and help food to move through the stomach more easily. However, there are side effects including diarrhea, anxiety, and drowsiness.
- Erythromycin - This is an antibiotic that will also stimulate stomach muscle contraction to push food through the stomach. Side effects do include diarrhea and building a tolerance if taken for a long time.
- Nausea and Vomiting Control - Other medications will help to manage nausea and vomiting symptoms, like prochlorperazine (Compro), ondansetron (Zofran), and promethazine (Phenergan).
Diet

A healthy diet can help to control symptoms and prevent complications.
How to Eat With Gastroparesis
Eating smaller meals throughout the day, rather than three large ones, helps to keep stomach contents moving along. That will also help your body to absorb nutrients from the food.
Chew your food more thoroughly. When you chew thoroughly, you increase the surface area of the food, which increases exposure to enzymes in saliva. Chewing also stimulates peristalsis, which pushes food through the gastrointestinal system.
After eating, it's best to sit or go for a walk. The upright position will help keep your food down and encourage digestion, rather than having food travel back up to your throat. It's not recommended to lie down for 2 hours after eating.
What to Eat With Gastroparesis
A low fat, low fiber diet is better for people with gastroparesis. This type of diet contains foods that are easier to digest and move through the digestive tract more easily.
Low fat diets are easier to digest because they contain fewer fats. Fiber slows down digestion so that food takes longer to pass through the stomach.
If you cook high-fiber fruits and vegetables longer than normal, it can help lower the fiber content.
Drink lots of liquids like water, juices, and sports drinks. Soups and puréed foods like applesauce are also good.
Taking a multivitamin supplement every day is important. These supplements provide vitamins and minerals that may be lacking in the diet.
Working with a nutritionist or dietician is helpful when trying to create a new diet plan. They can give you tips about how to eat healthier and what types of foods work well together for better digestion.
What Foods to Avoid With Gastroparesis
Avoid high-fat and high-fiber foods. High-fat foods will slow down digestion and high-fiber foods don't digest easily. That includes fried foods, fatty meats, greasy sauces, and spicy foods.
Avoid caffeine, alcohol, carbonated drinks, and chocolate. Avoid foods that cause bloating, gas, or cramping.
Try not to eat too much at one time because it causes discomfort and slows down digestion.
Acupressure Therapy
Acupressure therapy uses pressure points on different parts of the body to treat various issues, including gastrointestinal conditions.
Acupressure is commonly used for gas and bloating relief. See our guide to gas and bloating pressure points to learn more - Acupressure Points for Gas, Bloating, and Stomach Pain.
Follow these steps to apply pressure and massage the various acupressure points:
- Locate the pressure point and apply firm pressure for 5 seconds.
- Slowly and gently massage the point for two minutes.
- Repeat the cycle a few times throughout the day for relief.
For gastroparesis symptom relief, these are the main pressure points to stimulate:
Stomach 36 (ST 36) - Zusanli or Three Mile Point

The Stomach 36 pressure point is located below the kneecap four finger widths down and one finger width to the outside of the shinbone.
Stimulating this pressure point can help relieve stomach pain and digestive issues. Massaging this point can also help to relieve nausea and stress.
Spleen 6 (SP 6) - Sanyinjiao

The Spleen 6 is located 3 finger widths above the top of the inside of the ankle.
Applying firm pressure and massaging this point will offer relief to gastrointestinal and digestive conditions. Stimulation at the pressure point will influence the lower abdomen and parasympathetic nervous systems.
It's also a good pressure point to gently massage before going to bed because it will help to calm the mind, relieve anxiety and stress, and help with insomnia. This point can also offer menstrual pain relief.
If you're pregnant, it's best to stay away from this pressure point because it can induce contractions and labor.
Conception Vessel 6 (CV 6 or REN 6) - Qihai or Sea of Qi

The Conception Vessel 6 acupressure point is found three finger widths below the umbilicus (belly button).
This is one of the key pressure points that will help to strengthen the body's core. Stimulating this point will help with gas, bloating, constipation, digestion, and other gastrointestinal conditions. It's also a good point for menstruation.
Conception Vessel 12 (CV 12) - Zhongwan

The Conception Vessel 12 pressure point is located four finger widths above the belly button (navel). This can be more sensitive than other points, so start more gently with the pressure.
Stimulating this point will help with bloating and gas, as well as gastrointestinal and digestive conditions.
Bladder 21 (B 21) - Weishu
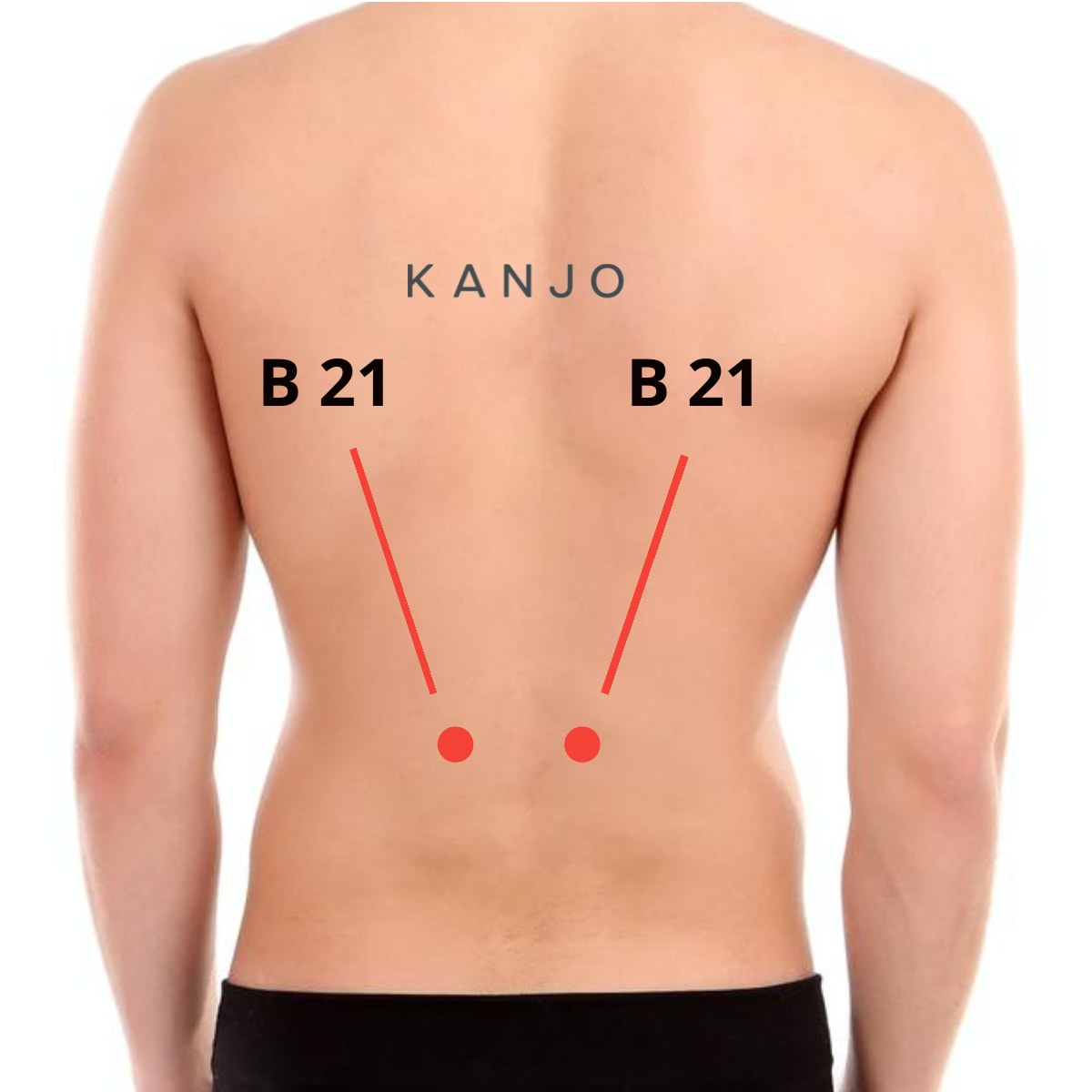
There are two Bladder 21 pressure points that are found 6 inches above the small of your back and 1.5 inches on the left and right sides of your spine.
Applying pressure and massaging these points will stimulate the abdominal organs to help relieve digestive issues like gas, bloating, and stomach pain.
Surgery
In some cases, surgery can be used as treatment for gastroparesis. There are two main surgeries that are performed: jejunostomy and gastric neurotransmitter.
Jejunostomy
This procedure involves creating an opening into the small intestine from the stomach. A jejunostomy tube (feeding tube) is placed in this opening.
Food and nutrients are inserted directly into the tube, so it goes around the stomach and directly into the small intestine where it is digested and absorbed by the intestines.
Jejunostomy is usually temporary for severe gastroparesis.
Gastric Neurotransmitter
A Gastric Electrical Stimulator (GES) is another option for treating gastroparesis. The device is implanted in the stomach and sends electrical impulses to stimulate nerves in the stomach.
The electrical stimulation helps improve symptoms such as nausea, vomiting, and abdominal pain. In one study, 97% of patients with a GES showed nausea and vomiting reduction.
Parenteral Feeding
Intravenous feeding (parenteral feeding) can also be used to treat gastroparesis. This involves inserting a feeding tube directly into a vein in your chest to feed you nutrients.
IV feeding is meant to be temporary for severe cases of gastroparesis.
Gastroparesis FAQs

What Is the Life Expectancy if You Suffer From Gastroparesis?
Gastroparesis by itself isn't life-threatening, but it will affect the quality of your life and lead to other conditions that can shorten your lifespan. It may cause dehydration, malnutrition, weight loss, fatigue, and poor nutrition.
How to Handle Flare-Ups of Gastroparesis?
If you have gastroparesis, there may be times when you experience a flare-up. These flare-ups can include nausea, vomiting, or abdominal pain. Depending on your symptoms, you can try different remedies to lessen the effects. Drink water to replace the lost liquids, try acupressure, and eat light foods.
Is Gastroparesis Curable?
Unfortunately, gastroparesis is not curable. You can only manage your symptoms by taking medications and following a healthy diet. People with gastroparesis can live long lives with proper management.
What Are the Symptoms of Slow Digestion?
The most common symptoms of slow digestion include feeling full quickly after eating a little, having hard stools, a bloated belly, abdominal bloating or pain, heartburn, vomiting, or nausea. If you notice any of these symptoms, see your doctor for a diagnosis to see what the issue is.
Do You Poop With Gastroparesis?
Gastroparesis is often associated with constipation because the stomach doesn’t empty properly. People who suffer from gastroparesis don’t always poop regularly because the food isn't moving through the digestive tract.
Is Gastroparesis Worse at Night?
Yes, it's possible that gastroparesis is worse at night. That's because the food you've eaten throughout the day could still be in your stomach, so all that undigested food has built up. When you go to bed, this extra food can cause more gas, bloating, and discomfort at night.
Do Probiotics Help Gastroparesis?
Probiotics can be beneficial to helping gastroparesis symptoms because they add good bacteria for better overall gut health. Probiotics will help the body better maintain healthy gut flora levels to help prevent bacterial overgrowth.
Sources:
- Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/gastroparesis/symptoms-causes/syc-20355787
- Cleveland Clinic: https://my.clevelandclinic.org/health/diseases/15522-gastroparesis
- Rare Diseases: https://rarediseases.org/rare-diseases/gastroparesis/
- WebMD: https://www.webmd.com/digestive-disorders/gastroparesis-digestive-disorders
- Healthline: https://www.healthline.com/health/gastroparesis
- Cedars Sinai: https://www.cedars-sinai.org/health-library/diseases-and-conditions/g/gastroparesis.html

Can a flare-up include, belching, bloating, and an appetite but experiencing nausea/heart burn?